EHR vs EMR: What are the key differences?

Discover the differences and similarities between electronic health records (EHR) & electronic medical records (EMR) to make informed healthcare decisions.
Do you think you can clearly define the difference between an electronic health records (EHR system, and an electronic medical records one? I’ve sometimes heard from clients that they think they’re two different terms for the same thing, but there are real differences. Getting a handle on the nuances between the two is more important than you might think. For example, consider the following differences:
- Scope of Information: EMR systems typically contain patient health information gathered in one healthcare organization, such as a hospital or clinic. EHR systems are designed to collect and store patient health information from multiple sources, including various healthcare organizations.
- Interoperability: EHR systems are built with interoperability in mind, allowing for the exchange of patient data across different healthcare providers, systems, and geographical locations. This interoperability is essential for providing seamless care to patients, facilitating communication among healthcare professionals, and ensuring continuity of care. That’s not to say EMRs aren’t capable of interoperating with other systems—in fact, according to an article from Webpt, “a specialty EMR with interoperable functionality may actually be better than a large-scale, generalist EHR for many providers—especially those in niche fields. With these types of systems, providers are able to maximize their workflows and processes with solutions that are well-suited to their specific needs—and still thrive in this new era of connected, collaborative care.”
- Regulatory Compliance: EHR systems are subject to more stringent regulatory requirements, such as those outlined in the Health Information Technology for Economic and Clinical Health (HITECH) Act and the Centers for Medicare & Medicaid Services (CMS) Promoting Interoperability Programs. These regulations aim to promote the adoption and meaningful use of EHR technology to improve healthcare quality, safety, and efficiency. Understanding these regulatory distinctions helps healthcare organizations ensure compliance and qualify for incentives or avoid penalties.
- Data Analytics and Population Health Management: EHR systems typically offer advanced analytics capabilities for population health management, clinical decision support, and quality reporting. These features help identify trends, monitor health outcomes, manage chronic diseases, and improve population health initiatives. Understanding this disparity helps healthcare providers leverage data-driven insights to enhance patient care, streamline operations, and achieve better health outcomes at both individual and population levels.
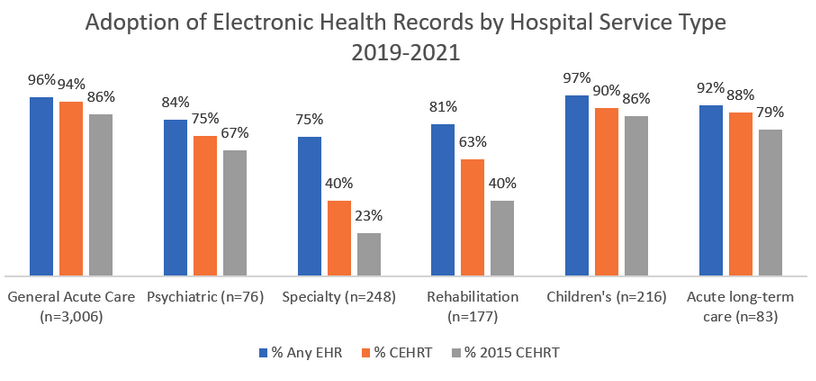
EHR and EMR adoption is becoming commonplace for healthcare providers, as seen in this chart from HealthIT.gov, which shows that a majority of providers have adopted some form of an electronic patient tracking system:
Understanding the differences between EHR and EMR systems is essential to make informed decisions about selecting, implementing, and leveraging electronic health records technology to improve patient care, operational efficiency, regulatory compliance, and population health management efforts.
Understanding the differences
Let’s delve deeper into a detailed comparison of EHR and EMR systems, focusing on their functionalities, interoperability, and data accessibility:
Functionalities
EMRs are digital versions of paper charts within a single healthcare organization. They contain patient medical and treatment histories, diagnoses, medications, immunization dates, allergies, and laboratory test results. EMRs are primarily used for diagnosis and treatment within the organization where they are implemented, but they also streamline workflows within the organization, such as appointment scheduling, prescription management, and clinical documentation. Additionally, EMRs often include tools for medical billing and coding.
EHRs are broader in scope and encompass health information from multiple healthcare organizations. They contain comprehensive patient health information, including medical history, diagnoses, medications, allergies, laboratory results, imaging reports, vital signs, progress notes, and treatments. EHRs support interoperability, allowing information exchange across different healthcare providers and settings. This also helps to facilitate care coordination among healthcare professionals by providing a centralized platform for accessing and sharing patient data. EHRs often include features for patient engagement, such as patient portals for appointment scheduling, secure messaging, and access to personal health records.
Interoperability
EMR systems are typically designed for internal use within a single healthcare organization. That means their Interoperability capabilities can be limited, making it challenging to exchange patient data with external systems or providers. Data exchange may rely on standard formats like HL7 (Health Level Seven) but may require customization and integration efforts. But that’s not to say EMR systems aren’t interoperable—in fact, many innovative solutions are just as functional for interoperability as large EHRs.
The distinction is EHR systems are built with interoperability in mind, aimed at enabling seamless data exchange among different healthcare organizations, systems, and stakeholders. They support interoperability standards, such as HL7, FHIR (Fast Healthcare Interoperability Resources), and CCD (Continuity of Care Document). EHRs facilitate health information exchange (HIE) initiatives, allowing for the secure sharing of patient data across organizational boundaries.
Data accessibility
Access to EMR data is typically limited to authorized users within the healthcare organization where the system is deployed. Data accessibility may vary based on user roles and permissions set by the organization’s administrators. Patients may have limited access to their medical records, often requiring requests through the healthcare provider or institution.
EHR systems prioritize patient data accessibility and empower individuals to access their health information securely. Patients can access their EHRs through online portals, mobile apps, or personal health record (PHR) platforms. EHRs support data exchange with external stakeholders, such as other healthcare providers, specialists, pharmacies, and public health agencies. Data accessibility in EHRs promotes patient engagement, self-management, and shared decision-making, leading to improved health outcomes and satisfaction.
Benefits of EMR and EHR systems
EHR and EMR systems in healthcare settings offer several key benefits that can significantly improve patient care, enhance communication between healthcare providers, and streamline administrative processes. Take a look:
Improved patient care
- Comprehensive Patient Information: EHR and EMR systems provide a centralized repository for storing patient health information, including medical history, diagnoses, medications, allergies, lab results, and imaging reports. This access helps healthcare providers to make more informed clinical decisions, leading to better patient outcomes.
- Clinical Decision Support: EHR systems often include clinical decision support tools that offer real-time guidance to healthcare providers based on evidence-based guidelines, best practices, and patient-specific data. These tools can help identify potential drug interactions, allergies, or preventive care opportunities, ultimately enhancing patient safety and quality of care.
- Remote Access and Telemedicine: Electronic records support remote access and telemedicine initiatives, allowing healthcare providers to deliver care beyond traditional clinical settings. Telehealth visits, remote monitoring, and virtual consultations enabled by EHR and EMR systems improve access to care, particularly for patients in rural or underserved areas.
Enhanced communication between healthcare providers
- Interoperability: EHR systems facilitate seamless communication and data exchange among healthcare providers across different organizations and specialties. Interoperable electronic records enable care coordination, care transitions, and collaborative decision-making, leading to more efficient and integrated patient care.
- Secure Messaging: Many EHR platforms include secure messaging features that enable healthcare providers to communicate securely within the system. Secure messaging streamlines communication workflows, reduces reliance on fax machines and paper-based communication, and ensures that sensitive patient information is protected.
Streamlined administrative processes
- Efficient Documentation: EHR and EMR systems automate and streamline documentation processes, reducing the time and resources spent on manual record-keeping tasks. Electronic documentation tools offer templates, shortcuts, and voice recognition capabilities that improve documentation efficiency while maintaining accuracy and compliance with regulatory requirements.
- Billing and Revenue Cycle Management: Electronic records integrate with billing and revenue cycle management systems, streamlining the billing process and reducing billing errors. Automated coding, charge capture, and claims submission functionalities improve billing accuracy, accelerate reimbursement cycles, and optimize revenue capture for healthcare organizations.
- Workflow Optimization: EHR systems support workflow optimization initiatives by standardizing clinical workflows, automating routine tasks, and providing insights into operational inefficiencies. Workflow optimization enhances productivity, reduces administrative burden, and allows healthcare providers to focus more on patient care.
Increased efficiency and accuracy in medical decision-making
- Data-driven Insights: EHR and EMR systems generate data-driven insights and analytics that inform medical decision-making and quality improvement initiatives. Advanced analytics tools help healthcare providers identify trends, monitor outcomes, and implement evidence-based practices, leading to more effective and personalized patient care.
- Clinical Alerts and Reminders: EHR systems can deliver clinical alerts and reminders to healthcare providers based on predefined criteria, such as medication reminders, preventive screenings, or follow-up appointments. These alerts improve adherence to clinical guidelines, enhance patient safety, and reduce the likelihood of medical errors.
Best practices
How can you best make use of these systems in practice? Here’s a few tips to help you focus your efforts:
Training and Education
Provide comprehensive training to all staff members on the functionalities and workflows of the EHR or EMR system. Offer ongoing education sessions to keep staff updated on system updates, new features, and best practices. Encourage staff to become proficient in using the system to optimize efficiency and accuracy in documentation and data management.
Data Management
Establish clear protocols and standards for data entry, documentation, and coding to ensure consistency and accuracy. Regularly review and update patient records to reflect the most current information, including diagnoses, medications, allergies, and test results. Implement data validation checks and quality assurance processes to identify and correct errors or inconsistencies in patient data.
Patient Engagement
Promote patient engagement by encouraging patients to access their health information through the patient portal or mobile app. Provide patients with educational resources and tools to help them understand their health conditions, treatment options, and preventive care recommendations. Use secure messaging features to facilitate communication between patients and healthcare providers, addressing questions, concerns, or medication refill requests promptly.
Interoperability and Health Information Exchange (HIE)
Participate in health information exchange (HIE) initiatives to facilitate seamless data exchange with external healthcare providers and organizations. Ensure compliance with interoperability standards, such as HL7 and FHIR, to support data exchange and integration with other systems. Collaborate with local or regional HIE networks to improve care coordination, transitions of care, and patient outcomes across care settings.
Regulatory Compliance
Stay informed about regulatory requirements and standards, such as HIPAA, HITECH, and CMS Promoting Interoperability Programs. Implement security measures, access controls, and encryption protocols to safeguard protected health information (PHI) and maintain compliance with privacy and security regulations. Regularly conduct audits and assessments to monitor compliance with regulatory standards and address any identified gaps or vulnerabilities.
Continuous Quality Improvement
Use EHR or EMR data analytics and reporting tools to monitor clinical outcomes, identify areas for improvement, and track performance metrics. Establish quality improvement initiatives focused on enhancing patient care, safety, and satisfaction based on data-driven insights. Foster a culture of continuous learning and improvement by encouraging feedback from staff and patients and implementing evidence-based practices to optimize healthcare delivery.
Data security
Data security is a critical aspect of EHR and EMR systems, given the sensitive nature of patient health information (PHI) stored within these electronic records. Safeguarding patient information, complying with privacy regulations, and implementing robust security measures are essential to protect the integrity and confidentiality of electronic health records. It’s a great help for maintaining compliance with HIPAA as well.
Taking the next step
The key differences between EHRs and EMRs lie in their scope, interoperability, and data accessibility. EHR systems encompass health information from multiple healthcare organizations, support interoperability for seamless data exchange, and offer patient access features. EMR systems, on the other hand, focus on patient information within a single organization and may lack interoperability and patient engagement functionalities.
Understanding these distinctions is crucial for healthcare providers and organizations. Choosing the right electronic records system can enhance patient care, streamline workflows, improve communication, and ensure compliance with privacy regulations.
We encourage you to check out our resources and reach out if you need more insight as to what kind of system will benefit you the most. Consulting with IT professionals, attending training sessions, and staying informed about industry trends and best practices can help maximize the benefits of electronic records while minimizing potential challenges and risks.
Rely on Kipu to keep you ahead of change.
Subscribe to Kipu for behavioral health news, updates, community celebration, and product announcements.




