Behavioral Health Revenue Cycle Management for Optimized Billing Processes

Build a Healthy Bottom Line with Kipu RCM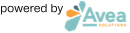
Navigating the intricate world of billing and revenue collection in behavioral health services is no small feat, given the complexity of workflows from pre-admission through post-discharge. Kipu’s Behavioral Health Revenue Cycle Management (RCM) offers a comprehensive solution, embedding essential workflows and payer requirements at each phase of the patient journey. This ensures claims are submitted accurately and expedited for payment, freeing your billing teams from the cumbersome manual processes and mundane tasks that hinder efficiency. Our addiction treatment billing software leverages automation and a powerful claim rules engine to boost cash flow, making it a game-changer for your practice.
In the behavioral health sector, the medical billing and coding process encompasses a series of meticulous steps, each with its own set of unique challenges and complexities. From accurately capturing patient information and services rendered to navigating the intricate payer requirements and coding standards, the process demands a high level of precision and expertise. This is where Kipu’s RCM services shine, offering not just a tool, but a partner in maximizing revenue and streamlining billing processes. Our system is designed to address the industry-specific challenges head-on, enhancing the overall efficiency and effectiveness of your revenue cycle management.
Integration with Kipu EMR transforms the billing workflow, saving valuable time and minimizing human error. With a single click, patient demographics and charges are seamlessly transferred to the billing software, streamlining the process from care to claim. Annually, Kipu RCM skillfully assists in submitting nearly 800,000 claims, demonstrating its capacity to handle the demands of the behavioral health industry with precision and efficiency.
Discover the difference expert RCM software can make in maximizing revenue and optimizing billing processes in the behavioral health industry. Kipu’s integrated solution not only tackles the unique challenges faced but also contributes significantly to the overall efficiency and effectiveness of revenue cycle management, ensuring your treatment facility can focus on what truly matters—providing exceptional patient care.
Key Components of Behavioral Health RCM Software
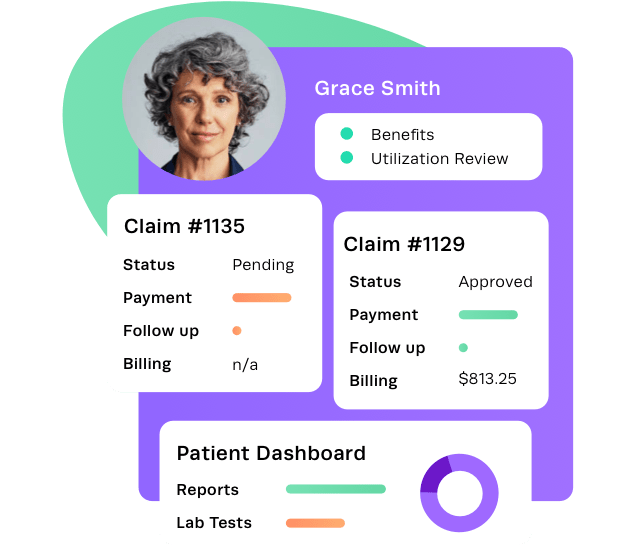
Simplifying the Process of Verifying Patient Eligibility and Benefits is Essential for a Smooth Patient Financial Journey and Easy Reimbursement
With our comprehensive Management Center, you can conveniently handle all aspects of eligibility and benefit verification in a single centralized location. Say goodbye to time-consuming tasks and enjoy streamlined operations that pave the way for a healthy revenue cycle.
Detailed coverage information
Obtain detailed coverage information in a user-friendly PDF format quickly and effortlessly through electronic eligibility checks, ensuring comprehensive coverage details are readily available.
Verification
Stay informed and prioritize important verification of benefit exceptions with the Management Center, enabling effective management of coverage issues that require follow-up.
Eligibility Check
Conduct real-time electronic eligibility checks for all active patients or set up automated schedules to run eligibility checks on existing clients at specified intervals using the batch eligibility feature.
Mastering Utilization Review (U/R) is Crucial for Minimizing the Gap Between Patient Treatment and Reimbursement
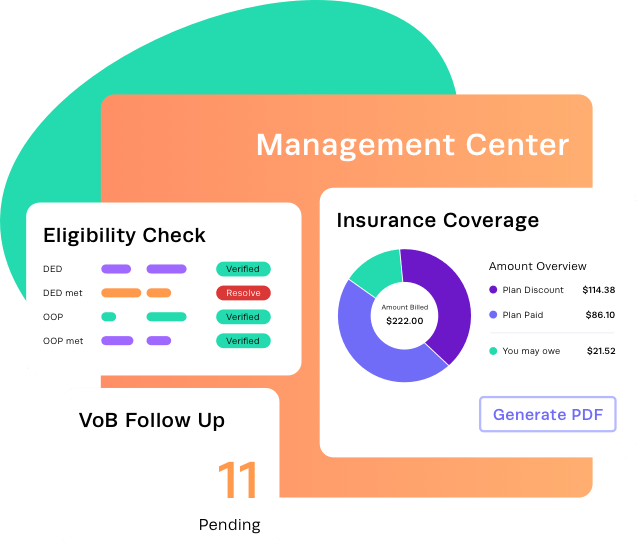
Our U/R Work Center empowers your staff’s U/R proficiency by providing a centralized hub for managing U/R plans. With color-coded alerts and task assignment features, you can easily prioritize and complete essential tasks. Our user-friendly system ensures that your facility stays updated with the latest authorizations, streamlining the U/R process for optimal efficiency.
Dashboard alerts
Prevent revenue gaps before they occur by staying informed with color-coded dashboard alerts for new, incomplete, and expired or soon-to-be-expired utilization reviews.
Authorization alerts
Keep on top of authorizations through proactive alerts, ensuring timely updates.
Utilization plans
Create Utilization Plans directly from the patient’s treatment episode or within the U/R Work Center for easy reference.
Task management
Assign and track tasks to team members for efficient follow-up on important items.
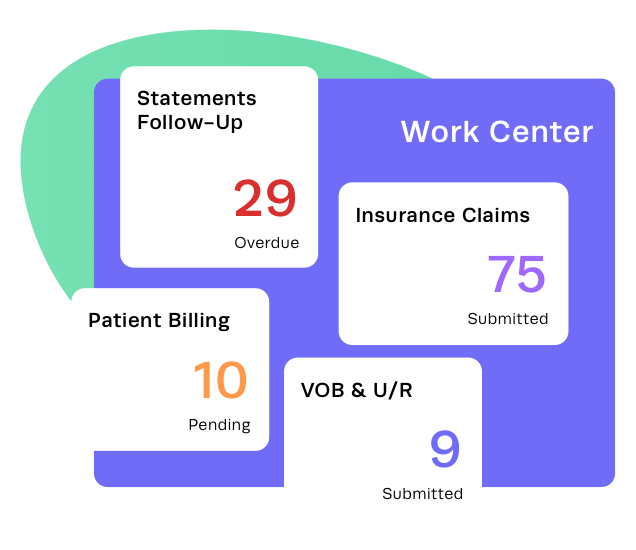
Patient Payments Don’t Need to Be a Barrier to Care With the Right Tools on Hand
With our electronic eligibility and verification of benefits tools, you’ll have already gained insights into patient responsibility, making the payment collection process even easier. From pre-admission to discharge, we provide collection alerts at the right moments during the patient journey, ensuring timely payment processing while delivering a smooth patient financial experience. To offer flexibility and convenience, we offer various payment options, including credit card and ACH payments, empowering patients to choose the method that suits them best.
Payment collection
Collect proper payment at any point in the patient journey—including pre-admission.
Payment reports
Reconcile bank deposits in a snap with the Patient Payment Report providing all payments and adjustments during a specified data range.
Payment options
Enhance convenience for both patients and your staff by accepting various types of payments— such as co-pays, co-insurance, deposits, and more—through our secure in-app credit card or ACH payment options.
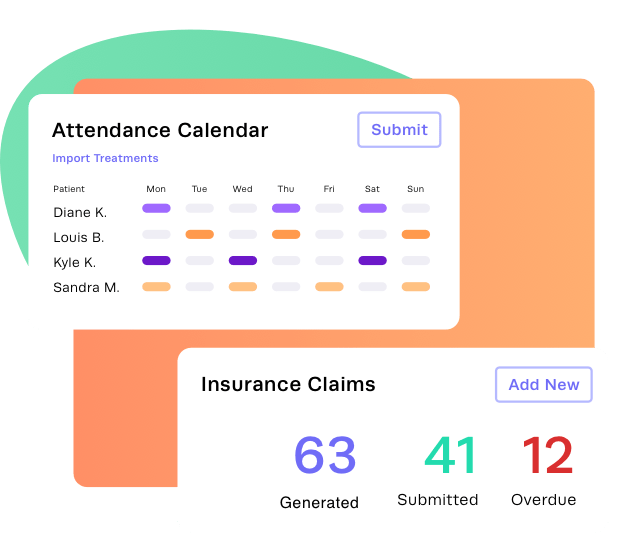
Automate Claim Creation with the Attendance Calendar
With this feature, you can effortlessly add and edit U/R required, standalone, and combined service sets for each treatment day, allowing for accurate tracking of patient progress and treatment. Enjoy the convenience of correcting and voiding claims with ease, reducing errors and ensuring prompt reimbursement. Experience streamlined treatment management and improved efficiency with our user-friendly Attendance Calendar.
Services rendered automation
Boost efficiency by automatically populating the Attendance Calendar with services rendered from the Kipu EMR or bulk importing treatments.
Claim automation
Generate claims automatically and with precision using the information from the Attendance Calendar.
Claims management
Correct and void claims quickly to enhance accuracy and ensure timely payment.
With Our Insurance Billing Solutions, You Can Have Peace of Mind Knowing That Your Billing is Always Accurate and Up to Date
Insurance billing is a challenging and time-consuming task. However, with our comprehensive software and trusted clearinghouse partners, you can eliminate the complexities of enrollments, automate payment posting, and streamline claims management.
Claims creation
Easily create claims and submit them to payers with information coming directly from the Kipu EMR and Attendance Calendar.
Payment insight
Review and analyze payments in bulk or dive into individual payments and provider-level adjustments for detailed insights.
Payer enrollments
Effortlessly enroll insurance providers with Kipu’s clear follow-up tasks for you to complete while we handle the necessary communication with the clearinghouse. Accelerate payment posting through automation when ERAs (electronic remittance advice) are received, and easily process insurance credit card payments or manually record payments when required.
Custom rules
Customize claim rules to ensure compliance with the requirements of even the most meticulous payers.
Payer management
Streamline the management of payer rates and fee schedules through simple uploads—saving time and effort.
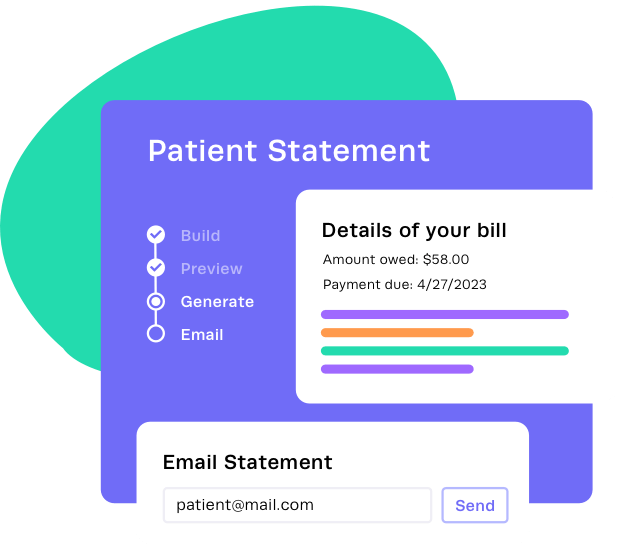
Provide the Seamless Financial Experience Your Patients Expect and Deserve Without Adding More Hassle For You
Our all-inclusive behavioral health revenue cycle management platform empowers you to efficiently manage every aspect of patient billing and collections from a single location. Experience the convenience of automated patient statement generation and seamless email delivery, putting your patient billing process nearly on autopilot.
Effortless statements
Generate easy-to-understand patient statements effortlessly for your entire organization or individual patients, with the ability to email them directly from the application in a matter of seconds.
Task management
Manage and prioritize follow-up tasks through color-coded alerts on the dashboard, allowing you to stay on top of outstanding payments and collections.
Payment options
Enhance your financial outcomes by offering convenient patient payment acceptance options that ensure a smooth and efficient payment process.
Automated follow-ups
Optimize your collections efforts with automated follow-up processes that help increase payment compliance and accelerate revenue recovery.
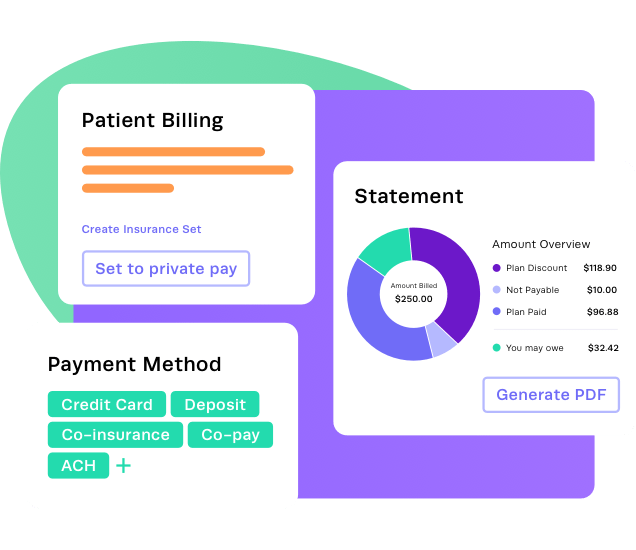
Optimize Self-Pay Revenue With User-Friendly Tools
Our easy-to-use RCM software offers convenient self-pay options that are readily available. With our user-friendly workflows, you can easily generate patient statements, collect payments at the right time, and effectively track and compare self-pay revenue to insurance revenue. Simplify the process and optimize your self-pay revenue with our seamless and efficient tools.
Statement transparency
Promote transparency with patients through customized comprehensive statements, enabling them to clearly understand the services provided.
Patient profiles
Build comprehensive self-pay patient profiles from the very beginning, allowing for accurate tracking and management of self-pay accounts.
Flexible payment options
Simplify payment collection with flexible options such as a securely stored credit card and ACH, ensuring a smooth patient journey including during pre-admission.
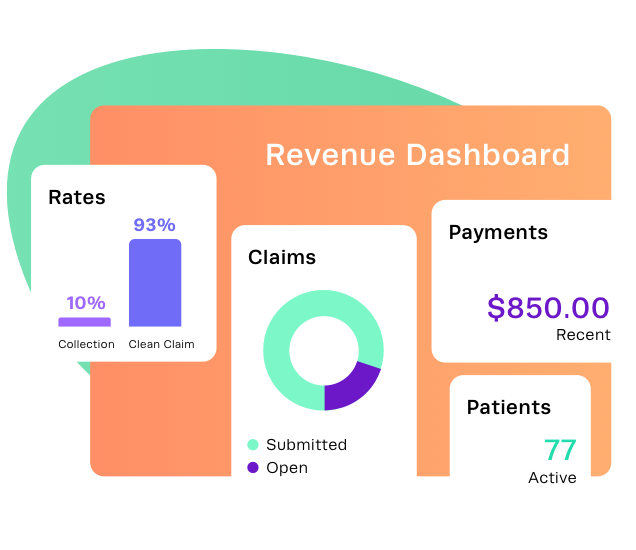
Access Critical Data and Gain Valuable Insights Into the Health of Your Revenue Cycle With Kipu RCM’s Reporting Dashboards
Quickly identify trends, potential issues, and critical metrics that impact patients, staff, and revenue. Our library of specialized reports is tailored to meet the needs of behavioral health businesses, and you can easily export data to Excel for further analysis. Make informed decisions with confidence and streamline your business operations with detailed reports and dashboards covering accounting, attendance, billing, utilization management, and more.
Instant insights
Accelerate your data analysis with pre-built reports specifically designed for addiction treatment and behavioral facilities, providing instant insights.
Comprehensive reports
Gain a comprehensive overview by accessing combined reports that include both insurance and self-pay data.
Efficient reporting
Customize reports to focus on the specific information you need and create report templates for consistent and efficient reporting.
Comparison snapshots
Compare data across different time periods—such as months, quarters, or years—with accurate and detailed period-close snapshot reports.
Kipu’s RCM solution provides expertise, insights, and analytics to move you forward.
Let’s chat more about how you can keep ahead with Kipu.