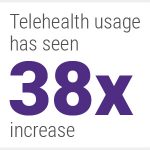
Post-COVID, telehealth usage has seen a 38x increase
COVID changed the behavioral treatment industry almost overnight. With social distancing disrupting traditional face-to-face consultations, telehealth is rapidly becoming a vital mode of care. What’s more, the demand for this new and complex form of treatment is coming at a time when the financial viability of treatment centers is under increasing pressure.
The shift to telehealth brings advantages. With less travelling and physical processing to undergo, telehealth can make life easier for patients. It can expand access to treatment in rural and remote areas. It could make treatment more affordable, especially with the potential proliferation of virtual-first health plans. It could also convince more people to enter treatment, given that logging into a virtual call is less daunting than travelling to a treatment facility.
Yet, reaping these benefits won’t be easy. Telehealth will also bring a number of challenges, which many treatment centers may struggle to circumvent. The consequences could be vast for both treatment centers and their patients. Telehealth means that centers are challenged to deliver much more complex care, demanding new levels of technological competence, regulatory compliance, and clinical flexibility. Given that not all insurers will reimburse telehealth treatment, understanding telehealth could be the difference between thriving and closing down.
Treatment Centers at the Forefront
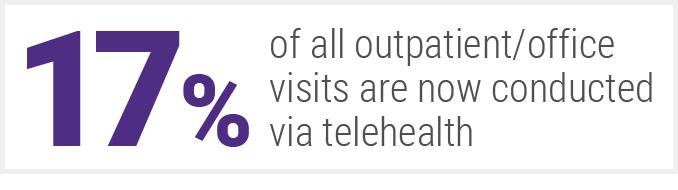
According to a 2021 report by McKinsey, “Telehealth: A quarter-trillion-dollar post-COVID-19 reality?” 17% of all outpatient/office visits are now conducted via telehealth. And treatment of substance abuse disorder represents the second-highest uptake of all medical fields, with only psychiatry demonstrating a greater adoption of telehealth. McKinsey estimates that providers are seeing 50 to 175 times the number of patients via telehealth than they did prior to the pandemic. So while the entire medical field is undergoing this transformational shift, behavioral care centers are finding themselves right at the forefront – where the most upheaval is likely to be experienced. While telehealth’s popularity has been precipitated by the pandemic, it’s likely to outlast it.
Telehealth is Here to Stay
The COVID-19 pandemic has accelerated telehealth adoption enormously. With social distancing, legal restrictions on travel, and enforced isolation, telehealth went from being a minority preference to an essential lifeline. Providers scrambled to offer care remotely, and overall, patients responded. The signs indicate that the shift to telehealth will be a long-term change. McKinsey’s report highlighted the ‘strong continued uptake’ and ‘favorable consumer perception’ of telehealth, concluding that it is more than a pandemic-induced fad.
So while telehealth might owe its sudden rise to the pandemic, it won’t be curtailed by COVID’s eventual conclusion. Adoption for behavioral treatment is strong, investment is quickly growing, and patients are becoming accustomed to being treated over the screen rather than in person. That’s why treatment facilities need to understand how best to offer, conduct, and process telehealth treatment. Much of the impact on patients isn’t fully known yet, but the implications could be vast.
Challenges for Patients
For patients, telehealth is an experiment full of unknown factors. Is care as effective via telehealth? How does it change group sessions as opposed to individual ones? What impact does it have on attendance rates? Even subtle differences could have profound implications. Behavioral treatment is sensitive to its environment. Group therapy, for example, is influenced by the subtle chemistry between the patients, as well as from patient to clinician. It’s unclear how things like dropped connections, poor clarity, and customized backdrops could affect telehealth treatment sessions, but it’s likely that their impact on outcomes will become clear very soon. Training clinicians to adopt best digital practices, as well as investing in hardware and software that enables better treatment, could make all the difference.
Some research is revealing that patients appear to be less satisfied with telehealth-only treatment. Vista Research Group conducted a study (via their Research Network of participating facilities) measuring the uptake of telehealth and its impact on patient satisfaction. They found that ‘patient satisfaction dropped measurably during the first few months of the pandemic’ – when telehealth-only treatment was at its peak. Around half of centers have opted to continue providing telehealth-only options, whereas the rest have formed hybrid treatments combining both telehealth and face-to-face care.
One of the patients surveyed in Vista’s investigation put it this way: “Going from regular meetings where there were bonds and physical embraces with other fellow addicts to the Zoom meetings made me feel more isolated and depressed”.
Another patient concurred: “The Zoom sessions are still challenging because we can’t hear everything people say. Some sessions feel like a waste of time”.
It’s important for treatment centers to identify telehealth’s potential impact on patient dissatisfaction, and to consider factors to mitigate it. Hybrid treatments could be the answer, but they must be implemented intelligently. How will the data from the telehealth sessions be integrated with the data gathered from face-to-face sessions, for example? There’s a lot to consider, but one thing is clear. In order to succeed, treatment centers must be in full control of their operations. Otherwise, they will struggle to implement telehealth in a way that does not compromise patient outcomes.
Challenges for Treatment Centers
The challenges around telehealth are both broad and deep. It isn’t yet clear, for example, whether the relaxation of restrictions precipitated by COVID-19 will continue. Many additional CPT codes were granted for telehealth coverage by the Center for Medical Services (CMS) in the 2021 physician fee schedule, but only on a temporary basis. For regulators, protecting privacy, governing the handling of private data, and maintaining robust cybersecurity must be weighed against the clear benefits of expanding access to treatment via telehealth.
Integration also needs to improve, especially regarding data flows between a myriad of providers. The telehealth ecosystem has expanded at such a rapid pace that neither centers nor insurers nor medical providers can keep up. With proliferation comes differentiation, and – unless interoperability can be adopted – incompatibility will result. There must be more guidance for treatment centers on how to select, adopt, and process telehealth treatment.
Embracing the Telehealth Revolution
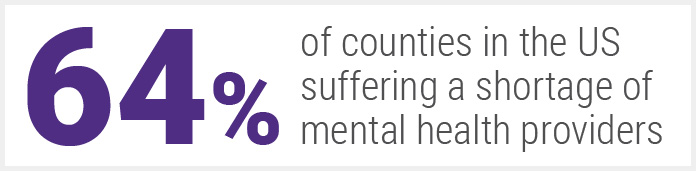
There are huge opportunities for behavioral health, if the industry embrace telehealth. With over two-thirds (64%) of counties in the US suffering a shortage of mental health providers, telehealth could enable existing facilities to expand and serve more patients – but only if they can do so safely, securely, and without compromising the quality of their care. In other words, they must master their operations and delivery before they can capitalize on these opportunities.
Ultimately, the benefits far outweigh the potential downsides for patients. For treatment centers, the picture is less clear. Telehealth is a more complex form of treatment, demanding new processes, methods, and technologies, thus placing more responsibilities upon treatment centers. Those with robust, integrated, and automated systems will most likely take the transition to telehealth in stride. But for those who are already struggling under the burden of increased regulation, administration, and lack of integration, telehealth is another daunting hurdle that threatens to topple their already-overwhelmed operation. So, as telehealth continues its meteoric rise, treatment centers must ensure that they get the basics right. Otherwise patients might find themselves going elsewhere – telehealth or no telehealth. Now is the time to transform the systems, operations, and processes upon which treatment centers rely, so that when it comes to offering more complex services like telehealth, centers have the capacity, confidence, and capability to do it effectively.
Find out how Kipu could help your treatment center to improve operations and deliver better treatment for patients – visit our site now.